Nature新见解:因为它们,CAR T免疫疗法才能有效治疗白血病
伦敦大学学院和大奥蒙德街儿童医院(GOSH)的科学家和临床医生研究了CAR T细胞疗法在儿童白血病中的有效性,发现了一小部分T细胞亚群在CAR T细胞疗法是否起作用中扮演了关键角色。
研究人员表示,“干细胞样记忆性T细胞(TSCM,stem cell memory T-cells)”对于从一开始就摧毁癌症以及进行长期免疫监测都至关重要,利用这种细胞可以改善CAR T治疗的设计和性能。
这项研究的主要作者Luca Biasco博士解释说:“在临床试验中,我们发现年轻的白血病患者取得了令人鼓舞的结果,但是目前尚不清楚为什么。从长远来看,CAR T细胞继续存在于某些患者中,阻止了癌症的复发,而其他患者则仍然处于复发的高风险中。”
“为了确保白血病治疗有效,任何CAR T细胞疗法都必须对人体识别和清除癌细胞的方式具有长期影响。在这项研究中,我们试图找到控制这些细胞的T细胞的来源和性质。”
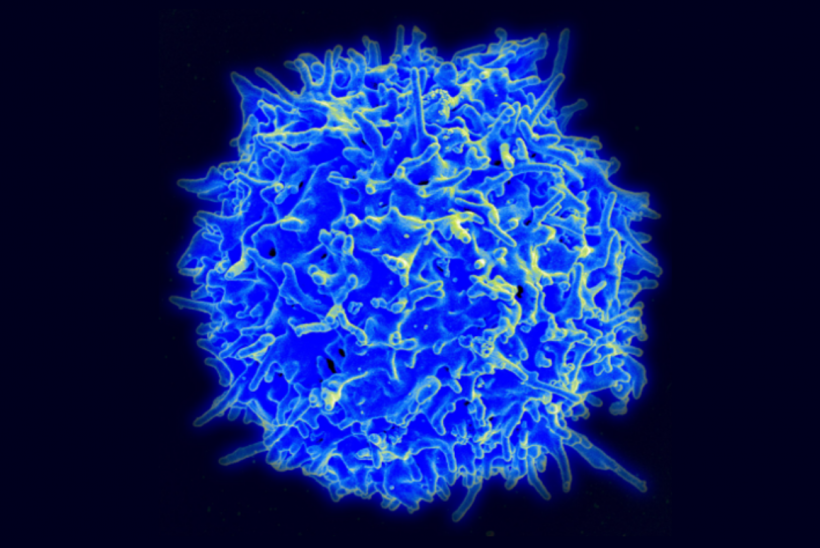
在CAR T治疗中,对免疫细胞(T细胞)进行了基因改造,使其表面上含有一种称为嵌合抗原受体(CAR)的分子,该分子可以特异性识别癌细胞。
研究人员评估了参与CARPALL I期研究的患者的CAR T细胞,该研究使用了由UCL癌症研究所和GOSH开发的称为CAT-19的新型CAR分子,用于治疗急性淋巴细胞性白血病这种儿童白血病。
研究小组比较了治疗后两年以上血液中仍可检测到CAR T细胞的患者的CAR T细胞,以及在治疗后一到两个月丢失了CAR T细胞的患者。
研究人员使用一种称为“插入位点条形码insertion site barcoding”的技术,能够在患者接受不同类型的CAR T细胞后研究其命运。
研究作者也是GOSH骨髓移植专家医师的Persis Amrolia教授分享道:“使用这种条形码技术,我们能够看到无论是在早期的抗白血病反应中,还是在后期的免疫监视中,TSCM都起着核心作用,机体都会识别并摧毁癌细胞。”
这表明,这种小的T细胞亚群对于治疗的长期成功至关重要。
研究人员说,这项工作表明,临床上可以测量患者进行抗白血病治疗后出现的CAR T细胞的类型,从而知道他们是否能够保存其CAR T细胞,避免复发。
Amrolia教授补充说:“这一新见解可能有助于我们改善CAR T细胞疗法,并确定哪些患者复发风险更高,并可能从CAR T细胞疗法后的干细胞移植中受益。”
Biasco博士补充说:“看到我们的新型条形码技术在研究CAR T细胞方面的应用,为我们揭示了这些细胞在送达患者后会发生什么变化的重要信息,这是非常令人高兴的。我们现在计划扩展该技术,我们在UCL建立了办事处,尝试在较大的患者群体中验证了这些发现。”
另外一位作者Martin Pule博士说:“这项研究为改善CAR设计和制造,改善CAR T细胞疗法的性能,实现了两者的结合开辟了新途径。”
Scientists and clinicians at UCL and Great Ormond Street Hospital (GOSH) studying the effectiveness of CAR T-cell therapies in children with leukaemia, have discovered a small sub-set of T-cells that are likely to play a key role in whether the treatment is successful.
Researchers say ‘stem cell memory T-cells’ appear critical in both destroying the cancer at the outset and for long term immune surveillance and exploiting this quality could improve the design and performance of CAR T therapies.
Explaining the study, published in Nature Cancer, lead author Dr Luca Biasco from UCL Great Ormond Street Institute of Child Health (UCL GOS ICH), said: “During clinical trials we have seen some very encouraging results in young patients with leukaemia, however it’s still not clear why CAR T-cells continue to be present in the long-term for some patients, stopping the cancer from returning, while others remain at a high risk of relapse.
“To ensure that a leukaemia treatment works any CAR T-cell therapy must have a prolonged effect on the way that the body recognises and removes cancer cells. In this study we tried to find the origin and nature of the T-cells that control these long-term responses.”
How does Car T therapy work?
In CAR T therapy, immune cells (T-cells) are genetically engineered to contain a molecule called a chimeric antigen receptor (CAR) on their surface which can specifically recognise cancerous cells.
Researchers assessed the CAR T-cells of patients involved in the CARPALL Phase I Study, which used a new CAR molecule known as CAT-19 developed between UCL Cancer Institute and UCL GOS ICH, for treatment in children with acute lymphoblastic leukaemia (ALL).
The team compared CAR T-cells from patients who still had CAR T-cells detectable in the blood more than two years after their treatment, with individuals who had lost their CAR T-cells in the one to two months post treatment.
Using a technique called ‘insertion site barcoding’, researchers were able to study the fate of different types of CAR T-cells in patients after they were given.
Corresponding author Professor Persis Amrolia, based at UCL GOS ICH and Consultant in Bone Marrow Transplant at GOSH, said: “Using this barcoding technique, we were able to see ‘stem cell memory T-cells’ play a central role both during the early anti-leukaemic response and in later immune surveillance, where the body recognises and destroys cancer cells.
“This suggests that this small sub-group of T-cells are critical to the long-term success of the therapy.”
Researchers say, this work indicates that the teams caring for patients could measure the types of CAR T-cells present after some someone has had their anti-leukaemia therapy, to gain an indication of whether they will be able to preserve their CAR T-cells into the future, avoiding relapse.
Professor Amrolia added: “This new insight may help us to improve our CAR T-cell therapy and work out which patients are at a higher risk of relapse and may benefit from a stem cell transplant after CAR T-cell therapy.”
Dr Biasco added: “It was extremely rewarding to see how the application of our new barcoding technology to study CAR T-cells is unveiling such important information about what happens to these cells after they are given to patients. We now plan to expand the technology we established at UCL and validate these findings in larger groups of patients.”
All research at Great Ormond Street is supported by the NIHR GOSH Biomedical Research Centre.